& to all a Good Night!!
Follow my adventures as I worked my way through an Emergency Medicine residency in Buffalo, NY. From So. Cal to Western New York, with stops in four states (Wisconsin, Illinois, Massachusetts, Minnesota) in between. It's been an incredible journey. Which continues on caldreamsquirrel.blogspot.com
New Blog
Continue the adventure at:
caldreamsquirrel.blogspot.com
25 December 2008
23 December 2008
Bookends
 Ok, so I had to work a shift at Buffalo General yesterday. It's one of the least favorite places for us to work because the system issues drive us crazy. To admit a patient takes a minimum of two phone calls. Most of the time it's three or four. And, the patients are generally sicker, have more medical problems, and can change on a dime.
Ok, so I had to work a shift at Buffalo General yesterday. It's one of the least favorite places for us to work because the system issues drive us crazy. To admit a patient takes a minimum of two phone calls. Most of the time it's three or four. And, the patients are generally sicker, have more medical problems, and can change on a dime.I call this entry "Bookends" because during my last two shifts, yesterday at "the General" and the prior one at ECMC, it seems my shift started and ended with similar cases....
I walked into the E.D. at the start of my ECMC shift on Saturday and was immediately directed by my attending to follow the incoming ambulance crew into Trauma One. We walked in to find a 70 year old gentleman with known dementia who had decided around 4 in the morning that he wanted a coffee from a local drive thru called Tim Horton's. The only problem with that is: 1 - it was 4 in the morning, 2 - he didn't take a coat, 3 - we had just had the season's highest snowfall in the days before, and 4 - had he wanted his usual frappacino he would have walked just a block down the road, but he turned in the opposite direction to the Tim Horton's located about 10 miles away.
He was found only about a block and half away from his home, but he had been out in the snow for several hours. He came in with frostbite to his hands and feet. His body temperature... 87.5 degrees F! Now, normal is 98.6 degrees. You begin to have heart arrythmias at around 91 or 92. The fact that he was actually talking to us, albeit just repeating over and over that he was cold, was a miracle.
We quickly stripped him down and placed him on top of and under warming blankets. We placed a catheter in his bladder to put in warm saline internally. I placed a central line so that warm saline could be infused as well. He was admitted to the burn center so that they could treat his hands and feet. I will check on his progress when I go back in tomorrow.
From there, the rest of the day flew by in a flurry of the usual standard fare of patients. About 45 minutes before the end of the shift, I was trying to wrap up my patients for the day when one of the EMT's asked me to triage a patient they were bringing in. It was a 40 something known opioid addict who was found in a snow drift.
I quickly directed them to Trauma Four where we learned that the patient had started throwing up after being given Narcan which is a reversal drug for opioid overdoses. When they were clearing his throat with suction, they noticed what looked like a gumball in the back of his throat. They couldn't remove it, so I quickly intubated him for a potential threatened airway. We didn't see a gumball, but there was a lot of irritated tissue and a foreign mass seen on CT. I'll find out what happened to him as well tomorrow.
Cookie break:
 So, I ended up working late. I had the next day off and then went to work at Buff General yesterday. One of the first patients we saw in the morning was a 65 year old gentleman who had gone outside to shovel the overnight snow. His wife saw him collapse and immediately called 911. Within two minutes BFD arrived and started CPR which continued until he got to the hospital.
So, I ended up working late. I had the next day off and then went to work at Buff General yesterday. One of the first patients we saw in the morning was a 65 year old gentleman who had gone outside to shovel the overnight snow. His wife saw him collapse and immediately called 911. Within two minutes BFD arrived and started CPR which continued until he got to the hospital.My senior and I went into the room, and I immediately took over and continued CPR. We worked on him for about 30 minutes while family started arriving. Unfortunately, we weren't able to get him back although we thought we had several times. My senior went to talk to the family, and I went back to work on the rest of my patients.
At the end of the day, after admitting a 43 year old who didn't want to comprehend that he'd had a heart attack and would have to, OMG, stop smoking and drinking and take medication for, um, the rest of his life because he'd had, oh yeah, A HEART ATTACK, I was signing out my patients to the on-coming senior when one of the patients that I'd had started having heart arrythmias.
I walked over with my attending and watched on the monitor as my patient's heart rhythm changed from something regular to something completely scary. His wife was just telling me that his AICD (automatic defibrillator) had just gone off. My patient was commenting that he'd been napping and had just had a rude awakening when all of a sudden he went into a deadly rhythm known as ventricular fibrillation. His heart started beating with no coordination at all.
We immediately gave him several external shocks as his AICD started firing off as well. Then he went into asystole, no heart activity at all. We started CPR and worked on him for about 10 minutes pushing a number of different drugs. He was intubated and we were able to get his heart rate stabilized and beating regularly. His pacemaker kicked in at that point and kept him going as well. I stayed late and placed a central line in him and watched as they took him up to the MICU.
I can see how far I've come, but I know there's still a long way for me to go. It's back to the County for me for the next two days. We'll see what kind of gifts Santa, via the EMT's, brings me for Christmas.

Labels:
AICD,
BGH,
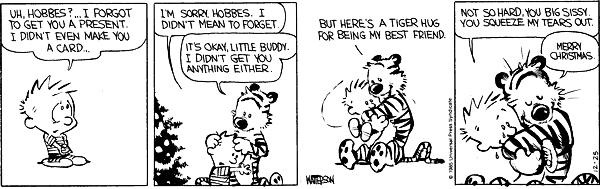
Calvin and Hobbes,
central venous line,
hypothermia,
intubation,
ventricular tachycardia
21 December 2008
Getting Out of the "Big" House
 The view from the ambulance ramp just after it started snowing. You can't see the trees and houses just across the drive.
The view from the ambulance ramp just after it started snowing. You can't see the trees and houses just across the drive.I think at some point I might have mentioned that we see a lot of the prison population at ECMC. One of the reasons being that we are the tertiary care center for a number of facilities. The other being that we have a very progressive telemedicine program which is connected to all of the correctional facilities in the state of New York.
We had a severe weather day on Friday when lots of snow (9 - 12 inches) was expected to fall over the course of about 12 hours. All of the schools were closed, and a lot of staff came in prepared to not be able to leave that night. The drive in was easy, but I had to spend about 20 minutes getting snow off my car (especially the 6 inches piled on the windshield) when I made the drive home 13 hours later. Luckily, I have a Jeep with 4 wheel drive and just rode over that foot and a half of snow piled up in front of it.

We kept expecting that it was going to be a light day. The snow started about 0900 and around noon, we were informed that there was a "no drive" directive out. However, we kept getting patients... mostly from the correctional facilities.
The complaints were legitimate enough that they warranted being seen, but not so critical that they needed to be seen "today."
Of course, one of the questions I always get asked when I can't provide a service on demand, such as a referral to a surgeon for an elective procedure, is "Is it because I'm wearing an orange jumpsuit?" I look at them, I look at the corrections' officer who is with them, then I look back at them and answer with a resounding, exasperated, "no!"
We never ask anything about our inmate patients. A lot of times, I am sure I don't want to know. I've treated lots of "accidental" falls that have resulted in broken noses, broken ribs, lot of cuts that need suturing, etc. I've treated STD's that have occurred. We have the frequent flyers who use their prior heart attack, asthma, HIV+ status, or seizure history to get out of jail for a while. We had one inmate with a psych history who was treated "Hannibal Lector" style since he was Hep C, HIV+ and liked to occasional spit and bite, or try to cause a needle stick incident when he was being treated.
Which reminds me: it's hard to get a physical exam on a patient wearing full jumpsuit with wrist and ankle cuffs attached to chains which are also wrapped around their midsection. But, for the most part, the CO's know what to do and start getting the pertinent body part ready for us to examine.
We also get a lot of new arrests. They either have just been arrested and have sudden chest pain or difficulty breathing and need a medical eval prior to being taken to jail. We've had the ones who made it to booking and then suddenly developed symptoms. We've had the hunger strikes, unwitnessed seizures, mysteriously injured jail-bound patients. I even had the patient with two days' nausea and vomiting that I had to now inform that she was pregnant. Bummer.
On Friday, all of the inmates were cleared and sent back to their respective facilities. A few looked disappointed that we couldn't admit them and get them out and into the real world... at least for a few more hours.
Labels:
correctional facilities,
ECMC,
Hannibal Lector,
Jeep Liberty,
snow storm
18 December 2008
Takotsubo Troubles
There's a medical condition in the literature known as Takotsubo Cardiomyopathy. It's basically broken heart cardiomyopathy where extreme grief or stress can actually lead to heart failure. It's been well documented in elderly widows who have chest pain or pressure at some point after losing their spouses. One of my favorite shows, "Scrubs," actually had the diagnosis as one of their story lines.
I think I might have written about the multitude of OD's we were seeing in the days following Thanksgiving (60 Hours), but lately it's seemed like I'm seeing a lot of depressed patients who come into the E.D. just for some companionship, or to have someone to talk to for a while. I did have two women who came in that made me think of Takotsubo's.
The first was a woman whose chief complaint was: chest pain. About 2 minutes after I started talking to her, I realized that her heartache was more of the emotional kind than the physical kind. She made a comment about all the "pressures" in her life at this time. When I pressed about them, she started crying and told me about how her fiance had died the year before, and how the holidays had always been a very special time for the both of them. They had been together for 8 years. She had family she wasn't really close to, and he had no one. They had each other.
She told me how she had seen him die right in front of her in a freak accident. One minute they were walking along, joking and laughing; the next, he had fallen down an embankment and died as a result of the fall. They had just gotten engaged and had not even gotten around to setting a date. I still had to work her up as a potential Acute Coronary Syndrome, but I ended up discharging her home with follow-up to counseling and psychiatry.
The second little lady came in this evening as I was trying to wrap things up at the end of my shift. Her chief complaint was "weakness." As I talked to her, she had some very non-specific symptoms: some nausea but no vomiting, some general feelings of "just being sick," and a feeling in her stomach that wasn't pain, and wasn't related to anything else. When I pushed her on it, she stated that she thought she might be lonely.
She lives in Senior Apartments. She doesn't like seeing ambulances coming and going at all hours. She's proud of her children and their accomplishments but calls them "work a holics" who don't have time to visit. She says her apartment is by the lake, but too much moisture which makes her bones ache. She said just being in the E.D. made her feel better. She told me that her physician told her that "loneliness will make you sick" and maybe that's all that is going on with her now.
When I signed her out at the end of my shift, I brought up Takotsubo's. My colleagues chuckled, but I'll think of this scene in "Scrubs" as I go to bed tonight; lying on a bed surrounded by three warm and purring kitties. Charles Schultz in "Peanuts" once said that "Happiness is a warm puppy." Too bad I can't write a prescription for a box of kittens or a warm puppy.
I think I might have written about the multitude of OD's we were seeing in the days following Thanksgiving (60 Hours), but lately it's seemed like I'm seeing a lot of depressed patients who come into the E.D. just for some companionship, or to have someone to talk to for a while. I did have two women who came in that made me think of Takotsubo's.
The first was a woman whose chief complaint was: chest pain. About 2 minutes after I started talking to her, I realized that her heartache was more of the emotional kind than the physical kind. She made a comment about all the "pressures" in her life at this time. When I pressed about them, she started crying and told me about how her fiance had died the year before, and how the holidays had always been a very special time for the both of them. They had been together for 8 years. She had family she wasn't really close to, and he had no one. They had each other.
She told me how she had seen him die right in front of her in a freak accident. One minute they were walking along, joking and laughing; the next, he had fallen down an embankment and died as a result of the fall. They had just gotten engaged and had not even gotten around to setting a date. I still had to work her up as a potential Acute Coronary Syndrome, but I ended up discharging her home with follow-up to counseling and psychiatry.
The second little lady came in this evening as I was trying to wrap things up at the end of my shift. Her chief complaint was "weakness." As I talked to her, she had some very non-specific symptoms: some nausea but no vomiting, some general feelings of "just being sick," and a feeling in her stomach that wasn't pain, and wasn't related to anything else. When I pushed her on it, she stated that she thought she might be lonely.
She lives in Senior Apartments. She doesn't like seeing ambulances coming and going at all hours. She's proud of her children and their accomplishments but calls them "work a holics" who don't have time to visit. She says her apartment is by the lake, but too much moisture which makes her bones ache. She said just being in the E.D. made her feel better. She told me that her physician told her that "loneliness will make you sick" and maybe that's all that is going on with her now.
When I signed her out at the end of my shift, I brought up Takotsubo's. My colleagues chuckled, but I'll think of this scene in "Scrubs" as I go to bed tonight; lying on a bed surrounded by three warm and purring kitties. Charles Schultz in "Peanuts" once said that "Happiness is a warm puppy." Too bad I can't write a prescription for a box of kittens or a warm puppy.
Labels:
kittens,
Peanuts,
Scrubs,
Snoopy,
Takotsubo's Cardiomyopathy
16 December 2008
Frequent Flyers
One of the things I don't think I've talked about in previous posts are the frequent flyers we get in the E.D. It seems like every E.D. has it's cast of known patients. Most of them, unfortunately, are either alcoholics brought in every several days by EMS after another drinking binge. Or they are the chronic drug seekers. Or patients with chronic back pain or sickle cell disease who need a shot of dilaudid to make it through to their next doctor's appointment.
A lot of ECMC's frequent flyers get greeted with a, "So, what's it going to take to get you out of the E.D. today, Johnny?" Sometimes, the discharge paperw ork is written at the same time as the dilaudid with a side of zofran order. Of course, we always worry about the possibility that one time a more serious problem is going to be missed.
ork is written at the same time as the dilaudid with a side of zofran order. Of course, we always worry about the possibility that one time a more serious problem is going to be missed.
I have been working at ECMC for the last two days. Along with the sundry assortment of the usual chest pains, shortness of breaths, etc, I have had a number of repeat customers. I don't mind seeing patients again, mostly to see that they have done better. However, I begin to obsess over what I might have missed the first time. Then, I begin to question the patients' true motives for returning to the E.D. Then I begin to get callous about these patients and wonder what exactly it will take to get them out of the E.D.
Of course, the management of the patient then has to be filtered through the attendings' own biases. Some attendings are of the treat and release type. Others make the patients go through a bit of bargaining before giving them their requested drug of choice. Still there are those that subject the patient to a new round of tests and queries, exhausting all diagnostic possibilities before resorting to giving the patient what they came in for. Finally, a patient might get admitted for "pain management."
One of my attendings today was more of the, "I have pain, they should be able to deal with theirs" variety. Made for quick turn arounds today.
Anyway, tomorrow is Grand Rounds Wednesday, then a stretch of three days before the weekend. We'll see what the weekend brings...!
A lot of ECMC's frequent flyers get greeted with a, "So, what's it going to take to get you out of the E.D. today, Johnny?" Sometimes, the discharge paperw
 ork is written at the same time as the dilaudid with a side of zofran order. Of course, we always worry about the possibility that one time a more serious problem is going to be missed.
ork is written at the same time as the dilaudid with a side of zofran order. Of course, we always worry about the possibility that one time a more serious problem is going to be missed.I have been working at ECMC for the last two days. Along with the sundry assortment of the usual chest pains, shortness of breaths, etc, I have had a number of repeat customers. I don't mind seeing patients again, mostly to see that they have done better. However, I begin to obsess over what I might have missed the first time. Then, I begin to question the patients' true motives for returning to the E.D. Then I begin to get callous about these patients and wonder what exactly it will take to get them out of the E.D.
Of course, the management of the patient then has to be filtered through the attendings' own biases. Some attendings are of the treat and release type. Others make the patients go through a bit of bargaining before giving them their requested drug of choice. Still there are those that subject the patient to a new round of tests and queries, exhausting all diagnostic possibilities before resorting to giving the patient what they came in for. Finally, a patient might get admitted for "pain management."
One of my attendings today was more of the, "I have pain, they should be able to deal with theirs" variety. Made for quick turn arounds today.
Anyway, tomorrow is Grand Rounds Wednesday, then a stretch of three days before the weekend. We'll see what the weekend brings...!
Labels:
ECMC,
frequent flyers,
sickle cell anemia
14 December 2008
California Dreamin'
I was going to call this blog entry "Ventura Highway" but I figured that not a lot of people would get the significance, other than the song by America. For some reason, during most of my trip back home to California this past week, I had that song running through my mind. Well, that and the title of this blog entry, "California Dreamin" which is another great song by the Mamas and Papas.
It's funny, but it seems that these last several trips home over the last several months have taken on a very nostalgic feel. Maybe because I'm returning to places I have been to over and over again. Maybe because I am sharing the travels with my new husband and my mother. My husband has never traveled in California, and my old places are new to him. My mother and I spend most of the road talking about this adventure, or that restaurant. How my uncle did this on one trip, or how we stopped for a picnic between those trees on another.

During this week, we did the day trip up north of Santa Barbara to a little Danish settlement of Solvang. The buildings are reminiscent of towns in Denmark. There are lots of shops that sell Danish imports; great restaurants that sell Danish fare, and now the more popular wine bars with tastings. Lot of local wineries, so some great samplings to be had.

The other thing that Solvang is famous for is its baked goods, especially its butter cookies. Tins and tubs of butter cookies. You can see them right now during the holidays when those paper-wrapped goodies are on every counter in the hospital. Darn blue tins.
The other part of the trip that I always enjoy is seeing the ocean again. They say that the Pacific has a memory, and I have a lot of memories of the Pacific. Especially driving along PCH (Pacific Coast Highway, Hwy 1). We pulled off the road in Malibu on our way back to catch the sunset. For a few brief moments we sat in silence watching the last of the days' final rays reach across the water.
 A sailboat made its way across the waters. As darkness fell, we pulled back on the road and continued our way home.
A sailboat made its way across the waters. As darkness fell, we pulled back on the road and continued our way home.
The rest of the week was filled with Christmas shopping with my mother, family affairs, and a lot of just plain old relaxing and lazing around the house. Not to mention eating just about all of my favorites while I was in town. Tomorrow back to the reality of the Emergency Department. Albeit, a bit more refreshed. More optimistic. Ready to carry forth.
Oh, and I lucked out just a bit: my upcoming rotation is a split month between the ED's at ECMC and Buffalo General, however, due to scheduling, I will only be doing two shifts at the General and the rest of my shifts at ECMC including Christmas Eve and Christmas Day. Sucks to work the holidays, but I anticipate a much pleasanter environment. We'll see!
It's funny, but it seems that these last several trips home over the last several months have taken on a very nostalgic feel. Maybe because I'm returning to places I have been to over and over again. Maybe because I am sharing the travels with my new husband and my mother. My husband has never traveled in California, and my old places are new to him. My mother and I spend most of the road talking about this adventure, or that restaurant. How my uncle did this on one trip, or how we stopped for a picnic between those trees on another.

During this week, we did the day trip up north of Santa Barbara to a little Danish settlement of Solvang. The buildings are reminiscent of towns in Denmark. There are lots of shops that sell Danish imports; great restaurants that sell Danish fare, and now the more popular wine bars with tastings. Lot of local wineries, so some great samplings to be had.

The other thing that Solvang is famous for is its baked goods, especially its butter cookies. Tins and tubs of butter cookies. You can see them right now during the holidays when those paper-wrapped goodies are on every counter in the hospital. Darn blue tins.
The other part of the trip that I always enjoy is seeing the ocean again. They say that the Pacific has a memory, and I have a lot of memories of the Pacific. Especially driving along PCH (Pacific Coast Highway, Hwy 1). We pulled off the road in Malibu on our way back to catch the sunset. For a few brief moments we sat in silence watching the last of the days' final rays reach across the water.
 A sailboat made its way across the waters. As darkness fell, we pulled back on the road and continued our way home.
A sailboat made its way across the waters. As darkness fell, we pulled back on the road and continued our way home.The rest of the week was filled with Christmas shopping with my mother, family affairs, and a lot of just plain old relaxing and lazing around the house. Not to mention eating just about all of my favorites while I was in town. Tomorrow back to the reality of the Emergency Department. Albeit, a bit more refreshed. More optimistic. Ready to carry forth.
Oh, and I lucked out just a bit: my upcoming rotation is a split month between the ED's at ECMC and Buffalo General, however, due to scheduling, I will only be doing two shifts at the General and the rest of my shifts at ECMC including Christmas Eve and Christmas Day. Sucks to work the holidays, but I anticipate a much pleasanter environment. We'll see!
04 December 2008
60 Hours
When I started my emergency medicine residency, I was told that all of our shifts are 12 hours long. Coming from a surgery residency where shifts can be 30 hours long, I was looking forward to the break. Having just spent the last five nights working a series of 12 hours shifts, I have realized that the hours add up pretty quickly.
 While I can't write about everything that happened over the last 60 hours, I can hit the highlights. I have also found that the more tired I am, the more surly I become with patients. After a brief 18 hours to adjust from night shift to day shift, I was back at work this morning. My body was telling me that it was nighttime and I should be sleeping. Caffeine does wonders for the sleepy mind.
While I can't write about everything that happened over the last 60 hours, I can hit the highlights. I have also found that the more tired I am, the more surly I become with patients. After a brief 18 hours to adjust from night shift to day shift, I was back at work this morning. My body was telling me that it was nighttime and I should be sleeping. Caffeine does wonders for the sleepy mind.
Anyway, what do I remember most about my last block of shifts:
- even pretty teenage girls from good families can be more troubled than you would think. I sewed up a 5 inch cut across her arm where she was "cutting" to hurt herself. It matched a series of other cuts that she had already put on her arm. This one was deeper than those, and I had to sew the wound closed in several layers and oversew a blood vessel that she had cut as well. Off to psych services, and probably alcohol rehab. She'd already lived more in 15 years than I had at 3o.
- the legend that people are more depressed around the holidays never showed more true than in this weekend after Thanksgiving. Our board shows the 20 rooms in the E.D. At least once per shift this weekend, there were 8 - 10 OD's, SIWL (self inflicted or suicidal ideation with laceration), rehab, depression, alcohol withdrawal, AMS (altered mental status), etc. on the board. It got so bad that I said that if I had to see one more suicidal patient or OD I was going to commit suicide. My senior actually called over to psych services to see if I could be committed for making a suicidal intent statement. They said yes, and that they would be more than happy to send security over to restrain me for a while. All in jest, but really... I was going crazy.
- there was a sale on car wrecks. Crash yours into someone else's and you both get seen for free!
- we had the first snowmobile accident of the year. No snow on the ground, he'd just had it tuned and wanted to hear it run... and it did, right into the building then flipped over on him. He had no injuries, luckily. We'll see how the rest of the season goes.
- for some reason, more stabbings are happening than shootings. They're a little hairier because you don't know just how far down the blade went. Bullets you worry about the path. Knives you're dealing with too many variables. We CT scan everyone. Oh, and marijuana is considered by some to be medicinal for post-traumatic stress following having been stabbed by your best friend who was high on "some pills" and thought you were suddenly out to get him. It's not.
- some attendings I get, some I just don't. Wonder what kind of attending I will be?
- even big strong 36 year olds die. Suddenly. We had one with a massive pulmonary embolism that died around 3 in the morning several nights ago. We worked hard to bring him back. Nothing would work. It affects the whole staff when something like that happens. Of course, I also had the 38 year old with end stage AIDS whose mother signed the "comfort measures" paperwork and then wouldn't let go of them. We all knew it was in the patient's best interest. I can't even begin to imagine the feeling of signing a paper that will limit the care your child receives. No matter the age, they are always your baby.
- which makes me salute all the mothers who brought their child to the ED for help and sat by their side while I explained what happens when you OD on soma, lortabs, alcohol, antidepressants; or while I sewed self-inflicted lac after lac; or who encouraged them to get help from Abuse Intervention Services because they "couldn't take it any more."
OK, it's late and I have one more shift before getting some time off... be happy! My ED patients have been so depressing lately.
 While I can't write about everything that happened over the last 60 hours, I can hit the highlights. I have also found that the more tired I am, the more surly I become with patients. After a brief 18 hours to adjust from night shift to day shift, I was back at work this morning. My body was telling me that it was nighttime and I should be sleeping. Caffeine does wonders for the sleepy mind.
While I can't write about everything that happened over the last 60 hours, I can hit the highlights. I have also found that the more tired I am, the more surly I become with patients. After a brief 18 hours to adjust from night shift to day shift, I was back at work this morning. My body was telling me that it was nighttime and I should be sleeping. Caffeine does wonders for the sleepy mind.Anyway, what do I remember most about my last block of shifts:
- even pretty teenage girls from good families can be more troubled than you would think. I sewed up a 5 inch cut across her arm where she was "cutting" to hurt herself. It matched a series of other cuts that she had already put on her arm. This one was deeper than those, and I had to sew the wound closed in several layers and oversew a blood vessel that she had cut as well. Off to psych services, and probably alcohol rehab. She'd already lived more in 15 years than I had at 3o.
- the legend that people are more depressed around the holidays never showed more true than in this weekend after Thanksgiving. Our board shows the 20 rooms in the E.D. At least once per shift this weekend, there were 8 - 10 OD's, SIWL (self inflicted or suicidal ideation with laceration), rehab, depression, alcohol withdrawal, AMS (altered mental status), etc. on the board. It got so bad that I said that if I had to see one more suicidal patient or OD I was going to commit suicide. My senior actually called over to psych services to see if I could be committed for making a suicidal intent statement. They said yes, and that they would be more than happy to send security over to restrain me for a while. All in jest, but really... I was going crazy.
- there was a sale on car wrecks. Crash yours into someone else's and you both get seen for free!
- we had the first snowmobile accident of the year. No snow on the ground, he'd just had it tuned and wanted to hear it run... and it did, right into the building then flipped over on him. He had no injuries, luckily. We'll see how the rest of the season goes.
- for some reason, more stabbings are happening than shootings. They're a little hairier because you don't know just how far down the blade went. Bullets you worry about the path. Knives you're dealing with too many variables. We CT scan everyone. Oh, and marijuana is considered by some to be medicinal for post-traumatic stress following having been stabbed by your best friend who was high on "some pills" and thought you were suddenly out to get him. It's not.
- some attendings I get, some I just don't. Wonder what kind of attending I will be?
- even big strong 36 year olds die. Suddenly. We had one with a massive pulmonary embolism that died around 3 in the morning several nights ago. We worked hard to bring him back. Nothing would work. It affects the whole staff when something like that happens. Of course, I also had the 38 year old with end stage AIDS whose mother signed the "comfort measures" paperwork and then wouldn't let go of them. We all knew it was in the patient's best interest. I can't even begin to imagine the feeling of signing a paper that will limit the care your child receives. No matter the age, they are always your baby.
- which makes me salute all the mothers who brought their child to the ED for help and sat by their side while I explained what happens when you OD on soma, lortabs, alcohol, antidepressants; or while I sewed self-inflicted lac after lac; or who encouraged them to get help from Abuse Intervention Services because they "couldn't take it any more."
OK, it's late and I have one more shift before getting some time off... be happy! My ED patients have been so depressing lately.
Labels:
AIDS,
AIS,
drug rehab,
MVC,
overdose,
suicidal ideations
28 November 2008
Black Friday...

My mother and I had a favorite tradition on Black Friday, the day after Thanksgiving. We would get up at 5 in the morning, dress warmly, and head off for the mall. We'd get the front line parking space and sit in the car waiting for 05:55 when we'd go stand at the door and walk in with the rest of the crowd.
We had our list. We'd do our shopping. And, at 08:30, we'd be done. While the rest of the cars were circling the parking lot, my mother and I would be allowing some lucky soul to take our spot as we headed off for breakfast. We might hit a specialty store or two after breakfast. Maybe go to a movie. Pick up something to snack on. Then come home and watch TV while eating leftovers from the night before.
We haven't done this in many years, but every Thanksgiving I still ask my mother if she'd like me to pick her up early to go shopping. She always laughs and asks what plane I'm landing on and is Starbuck's going to open early as well.
This year, I shared my Thanksgiving with family and friends, not my family and not my friends, but nonetheless, a warm loving atmosphere and good food throughout.
I do want to share a poignant vignette shared by one of my attendings yesterday. He stated that they had received a small child in cardiac arrest. The E.D. staff did their best, but there was no resuscitating the child. The family was in hysterics, and this increased as more family members arrived. The child was the youngest of three. It appeared to be a SIDS death.
The family stated that they had never heard of "Back to Sleep," and that the child was always placed to sleep on their stomach, covered by blankets. They didn't know any other way.
My attending stated the obvious, that a child's death is always hard on the staff. He shared that the way he dealt with it was by personally carrying the child down to the morgue. Which he did with this child. No cloth-covered gurney for these smallest of patients.
Tonight I'll be going in for a string of overnight shifts, and I'll be hoping that we're not "in the black" in the E.D. We'll see.
Labels:
Back to Sleep,
Black Friday,
SIDS,
Starbuck's
26 November 2008
Permanent Ink
I can remember as a teenager having my mother tell me repeatedly that decisions that I made came with consequences. This continued through college as she reminded me on a weekly basis that only I was responsible for my actions. In light of this, I was often not a spontaneous person, and in some ways, this has continued into my adult life. Take tattoos for example...
I always thought about getting a tattoo. The fun was in trying to decide what to get and where to put it. I remember in the first season of "Road Rules" one of the contestants who was a pre-med student got a tattoo of Kermit the Frog wearing a stethoscope on her hip. I thought that was kind of cool, especially when I got into med school. But then, I started thinking... what would that tattoo look like when I was 80? Would that still be cool?
to get and where to put it. I remember in the first season of "Road Rules" one of the contestants who was a pre-med student got a tattoo of Kermit the Frog wearing a stethoscope on her hip. I thought that was kind of cool, especially when I got into med school. But then, I started thinking... what would that tattoo look like when I was 80? Would that still be cool?
I trained at the V.A. during med school, so I had a great reference of tattoos as the WWII vets were mostly my patients. Following them, the Korean War and Vietnam Vets. A lot of them tattooed. You get to see the effects of time. So I continued to ponder.
As a fourth year medical student working one of my first shifts on my E.D. rotation, I remember a patient who came in. She was in her 80's and as I examined her, I noticed that her tattoos seemed especially bright. I commented to my senior resident, and they too wondered how the tattoos could have stayed so bright all of these years. Finally, before discharging her, I asked her about her tattoos. She smiled as she held out her arms. She told us that she had always wanted to get a tattoo, but that her husband had always been opposed. She said that when he died, about a year later she got her first tattoo. She now had her second. And, this had been within the last two years.
I was thinking about my own permanent ink fancies recently when I had a young female patient who came in with a complaint of "bloody urine." After a few minutes of discussion, "bloody urine" turned into abdominal pain, then she got teary as she described that she was really having pelvic pain. As in most cases, I asked about her sexual activity, and she admitted that she had a single boyfriend but that they didn't use protection because she was trying to get pregnant.
I went through my usual abdominal exam, noting a fresh new tattoo that started above her bikini line and wrapped around her waist. I then explained that I would have to do a pelvic exam because she could have an infection causing her problems. She became more teary as I performed the pelvic, and it became clear that she was having cervical motion tenderness, one of the signs for pelvic inflammatory disease, a process most often caused by an STD.
She started to cry as I explained what I felt was causing her pain, what medications I would be giving to her, and further instructions for her care. She then admitted that her boyfriend had cheated in the past, and she was feeling very stupid because she had just gotten the tattoo. That's when I took a second look and noted a name as part of the design. It's not my place to counsel patients on how to lead their lives, but I silently hoped that the ink would be the only consequence of her relationship with this other person.
I still think about tattoos from time to time... maybe when I'm 80. Now, where would I put it?? Where are yours?

I always thought about getting a tattoo. The fun was in trying to decide what
 to get and where to put it. I remember in the first season of "Road Rules" one of the contestants who was a pre-med student got a tattoo of Kermit the Frog wearing a stethoscope on her hip. I thought that was kind of cool, especially when I got into med school. But then, I started thinking... what would that tattoo look like when I was 80? Would that still be cool?
to get and where to put it. I remember in the first season of "Road Rules" one of the contestants who was a pre-med student got a tattoo of Kermit the Frog wearing a stethoscope on her hip. I thought that was kind of cool, especially when I got into med school. But then, I started thinking... what would that tattoo look like when I was 80? Would that still be cool?I trained at the V.A. during med school, so I had a great reference of tattoos as the WWII vets were mostly my patients. Following them, the Korean War and Vietnam Vets. A lot of them tattooed. You get to see the effects of time. So I continued to ponder.
As a fourth year medical student working one of my first shifts on my E.D. rotation, I remember a patient who came in. She was in her 80's and as I examined her, I noticed that her tattoos seemed especially bright. I commented to my senior resident, and they too wondered how the tattoos could have stayed so bright all of these years. Finally, before discharging her, I asked her about her tattoos. She smiled as she held out her arms. She told us that she had always wanted to get a tattoo, but that her husband had always been opposed. She said that when he died, about a year later she got her first tattoo. She now had her second. And, this had been within the last two years.
I was thinking about my own permanent ink fancies recently when I had a young female patient who came in with a complaint of "bloody urine." After a few minutes of discussion, "bloody urine" turned into abdominal pain, then she got teary as she described that she was really having pelvic pain. As in most cases, I asked about her sexual activity, and she admitted that she had a single boyfriend but that they didn't use protection because she was trying to get pregnant.
I went through my usual abdominal exam, noting a fresh new tattoo that started above her bikini line and wrapped around her waist. I then explained that I would have to do a pelvic exam because she could have an infection causing her problems. She became more teary as I performed the pelvic, and it became clear that she was having cervical motion tenderness, one of the signs for pelvic inflammatory disease, a process most often caused by an STD.
She started to cry as I explained what I felt was causing her pain, what medications I would be giving to her, and further instructions for her care. She then admitted that her boyfriend had cheated in the past, and she was feeling very stupid because she had just gotten the tattoo. That's when I took a second look and noted a name as part of the design. It's not my place to counsel patients on how to lead their lives, but I silently hoped that the ink would be the only consequence of her relationship with this other person.
I still think about tattoos from time to time... maybe when I'm 80. Now, where would I put it?? Where are yours?

Labels:
cervical motion tenderness,
STD's,
tattoos
22 November 2008
And, Now a Word From Our Sponsor...

I am going to say thank you to Donna at "Dust Bunny Protector" who awarded me the Marie Antoinette Award! It is given to people who we feel blog about "Real Life."
I started my blog in order to keep in touch with family and friends since I have been moving all over the country for the last 5 years. What I never expected was to make a whole new circle of friends who also blog. I really like coming home and reading about others' happenings.
I tried to find people who hadn't been nominated previously, and I hope you enjoy my choices as much as I enjoy reading them:
In no particular order:
Jeanie at "Genii in the Lakes"
Lisa at "Life on a Bison Farm"
Bethe at "Palm Harbor"
Winivere at "Woman in the Glass Box"
Frankie and Bella at "Twin Speak"
Betty at "A Corgi in Southern California"
and
De at "Where Do I Go From Here?"
Thank you for sharing a little piece of yourself and making all our lives just a little better!
Veronica
Labels:
blogging,
friendship,
Marie Antoinette Award
20 November 2008
And Now, Back to the Drama
I think I have mentioned on several occasions that one of the things I like most about working in the E.D. is the patient's back story. Their presenting complaint for the most part is routine, but the way they came to be in the E.D. usually is interesting. That's why I like ECMC. Patients there are not boring by any respect. Every day is like a soap opera; there's a plethora of drama for everyone to enjoy. And, it's played out right in front of you.
 Dx: Sickle Cell Crisis - "I think I am dehydrated because I have been drinking anything I can get my hands on because I am upset about my fiancee who got really sick from her diabetes and is now in a coma, and I drink from the time I get home from seeing her until I can't drink any more. And, I am changing doctors and my current doctor only gave me enough pills for a few days because they didn't know me, and now I am out of my oxycontin's and dilaudids, and now I am having a lot of pain, and I think I need a shot of something."
Dx: Sickle Cell Crisis - "I think I am dehydrated because I have been drinking anything I can get my hands on because I am upset about my fiancee who got really sick from her diabetes and is now in a coma, and I drink from the time I get home from seeing her until I can't drink any more. And, I am changing doctors and my current doctor only gave me enough pills for a few days because they didn't know me, and now I am out of my oxycontin's and dilaudids, and now I am having a lot of pain, and I think I need a shot of something."
Dx: Constipation - "I've been having abdominal pain for the last two months, and I've been to three different hospitals. My doctor won't even see me because she's only available on Mondays, and I was having abdominal pain, but I didn't have severe pain until today, and I knew that I couldn't wait until Monday, but then she wouldn't see me anyway because I always have to go see the nurse practitioner, and I never get to see the doctor." Why didn't you go back to the last hospital that saw you and has all your tests and records? "Well, I didn't like them there. They told me that nothing was wrong, and that I was just constipated and then they admitted me and then I felt better but then my doctor didn't work there so then I wouldn't have my own doctor, and this pain is so bad and I didn't want to wake up my brother because he sleeps in the room above me but he was so worried about me and what are you going to do to fix me?"
Dx: 4th metatarsal fracture - "Well I was fighting this girl and then she suddenly came out and stepped on my foot, and I haven't been able to walk on it ever since." Well, how have you been getting around? "I've had to crawl on the floor."
Dx: Overdose and suicidal ideations - "Well, one of my kids had a scratch so someone called CPS, and then they said because of the bruises that I would have to go to court, and then my husband said that (mumbles something incoherently) so then I decided that I couldn't live in a world without my children and I took a ll the pills."
ll the pills."
Dx: Multiple stab wounds - "I was fighting with this girl and then all of a sudden I felt this pain, and then I realized that I was bleeding and I couldn't believe that she would do that."
Oh... and the Award for highest blood sugar I've ever seen in a fully conscious patient goes to my homeless man who presented with a blood sugar of 1048. Yeah, that's right! Four digit blood sugar.(btw normal is around 100, most doctors recommend diabetics keep theirs below 160).
And, in my "Art Imitates Life" section: Tonight's episode of Grey's Anatomy had a storyline where one of the doctors Callie suffers a broken nose after getting clocked by the elbow of a patient... during a code today, I was placing a central line in the patient's femoral artery (in the thigh) when I bent over to get something from the kit I had to place on a chair. I was just about to turn back to the patient when one of the nurses toward the head of the bed turned suddenly and clocked me with her elbow. Not enough to daze me, but I did have to suffer through CT and subdural jokes for a part of the shift.
You have to watch out... life moves pretty fast in the E.D. Oh. yeah!
So lets get started on today's episode of "As the E.D. Turns." Questions I asked the patient are in red.
 Dx: Sickle Cell Crisis - "I think I am dehydrated because I have been drinking anything I can get my hands on because I am upset about my fiancee who got really sick from her diabetes and is now in a coma, and I drink from the time I get home from seeing her until I can't drink any more. And, I am changing doctors and my current doctor only gave me enough pills for a few days because they didn't know me, and now I am out of my oxycontin's and dilaudids, and now I am having a lot of pain, and I think I need a shot of something."
Dx: Sickle Cell Crisis - "I think I am dehydrated because I have been drinking anything I can get my hands on because I am upset about my fiancee who got really sick from her diabetes and is now in a coma, and I drink from the time I get home from seeing her until I can't drink any more. And, I am changing doctors and my current doctor only gave me enough pills for a few days because they didn't know me, and now I am out of my oxycontin's and dilaudids, and now I am having a lot of pain, and I think I need a shot of something."Dx: Constipation - "I've been having abdominal pain for the last two months, and I've been to three different hospitals. My doctor won't even see me because she's only available on Mondays, and I was having abdominal pain, but I didn't have severe pain until today, and I knew that I couldn't wait until Monday, but then she wouldn't see me anyway because I always have to go see the nurse practitioner, and I never get to see the doctor." Why didn't you go back to the last hospital that saw you and has all your tests and records? "Well, I didn't like them there. They told me that nothing was wrong, and that I was just constipated and then they admitted me and then I felt better but then my doctor didn't work there so then I wouldn't have my own doctor, and this pain is so bad and I didn't want to wake up my brother because he sleeps in the room above me but he was so worried about me and what are you going to do to fix me?"
Dx: 4th metatarsal fracture - "Well I was fighting this girl and then she suddenly came out and stepped on my foot, and I haven't been able to walk on it ever since." Well, how have you been getting around? "I've had to crawl on the floor."
Dx: Overdose and suicidal ideations - "Well, one of my kids had a scratch so someone called CPS, and then they said because of the bruises that I would have to go to court, and then my husband said that (mumbles something incoherently) so then I decided that I couldn't live in a world without my children and I took a
 ll the pills."
ll the pills."Dx: Multiple stab wounds - "I was fighting with this girl and then all of a sudden I felt this pain, and then I realized that I was bleeding and I couldn't believe that she would do that."
Oh... and the Award for highest blood sugar I've ever seen in a fully conscious patient goes to my homeless man who presented with a blood sugar of 1048. Yeah, that's right! Four digit blood sugar.(btw normal is around 100, most doctors recommend diabetics keep theirs below 160).
And, in my "Art Imitates Life" section: Tonight's episode of Grey's Anatomy had a storyline where one of the doctors Callie suffers a broken nose after getting clocked by the elbow of a patient... during a code today, I was placing a central line in the patient's femoral artery (in the thigh) when I bent over to get something from the kit I had to place on a chair. I was just about to turn back to the patient when one of the nurses toward the head of the bed turned suddenly and clocked me with her elbow. Not enough to daze me, but I did have to suffer through CT and subdural jokes for a part of the shift.
You have to watch out... life moves pretty fast in the E.D. Oh. yeah!
Labels:
constipation,
CPEP,
diabetic ketoacidosis,
ECMC,
overdose,
SCC
19 November 2008
The Boy and Girl Who Cried "Wolf"
 There are some patients that drive you crazy. Usually, they are the ones that come into the emergency department with a "I've had chest pain/cough/stomach pain/leg pain/back pain, etc for the last 6 weeks/months/etc. and I thought I should have it checked out." When you ask if they've ever talked to their primary physicians about the problem, they say "I forgot," "He's looked into it and hasn't found anything yet," or "No, I was going to mention it on my next visit, but I thought I should get it checked out today."
There are some patients that drive you crazy. Usually, they are the ones that come into the emergency department with a "I've had chest pain/cough/stomach pain/leg pain/back pain, etc for the last 6 weeks/months/etc. and I thought I should have it checked out." When you ask if they've ever talked to their primary physicians about the problem, they say "I forgot," "He's looked into it and hasn't found anything yet," or "No, I was going to mention it on my next visit, but I thought I should get it checked out today." It's hard not to discount those patients. Not to be mean, but seriously, like we always ask, "And, what about today made it so bad you had to come to the Emergency Department to be seen?" Two patients that I saw during my last shifts at Suburban are good examples of how even the simplest cases can surprise you.
We'll call the first patient Frank. Frank is around 72 and has dementia. He also had a heart attack about 10 years ago, underwent bypass surgery, and since then has complained on a regular basis about having chest pain. He was brought into the ED in the morning after having been found on the floor of his board and care facility lying in front of the elevator. He told paramedics that he didn't feel well and needed to lie down.
His daughter was called, and he complained to her about the chest pain. She told him that they would "go out to lunch" which she later told me was her way of "distracting him" from his usual rant about having chest pain. She explained that he had been evaluated time and time again for complaint about chest pain, and that all of the tests had been negative so far.
Still, he insisted on coming to the ED, and since EMS had already been called, they brought him in. So, we did our thing, evaluating him for the "chest pain" we assumed he didn't have, and expecting to discharge him after talking to his primary care physician. The first EKG didn't look very suspicious but still had some changes that made it just enough dissimilar to a prior EKG that we were more concerned than previously thought.
You can guess what was happening... his next EKG showed a major heart attack, and an EKG taken about 15 minutes later was worse still. We immediately contacted cardiology, and the patient was transported to another hospital to get angiography. When I called later that same day, a colleague told me that the patient was in the cardiac care unit. I'll find out tomorrow how he did. Needless to say, the daughter felt guilty, we felt guilty, and the patient almost suffered because of it.
The next patient we'll call Thelma. I saw Thelma on my last morning at Suburban. She is a sweet 80 year old lady who came into the "non-urgent" part of the E.D. that I picked up because I wanted an easy last day. Her complaint "chest pain" was classified a "green" not urgent because in triage she related her chest pain to her reflux disease and not as a cardiac issue.
When I talked to her, she was telling me that she'd had the pain for years, that her primary care physician had done multiple tests for it, and that this morning it didn't hurt any more or less than usual, but that she just thought she should "have it checked out." I asked when she'd last seen her doctor, Thelma told me she'd just seen him a few weeks earlier. When I asked if she had told him about her "chest pain" she said that she'd forgotten, but that he had been treating her for her reflux for years.
I went to my attending and told him that I didn't think she really had anything wrong with her. He asked what I wanted to do. I told him, that I really didn't want to do anything, but that we probably should just get a chest X-ray, EKG, and give her something for her reflux. It was an easy morning so far, so he said, "OK."
The EKG was not very exciting. I probably spent about another hour running around seeing other people before I had a chance to look at her chest X-ray. I took a look at it and quickly called my attending over. We both looked at it, and I went over to the computer to see if there was another X-ray to compare it to. Her last one had been in 2001, and there was nothing on the film viewer. All I had was the report. It was negative.
Her chest X-ray now showed a large mass in her lung. My attending and I shook our heads and both immediately agreed that she needed a CT scan of her chest. I told her we had seen a spot on her X-ray and just wanted to evaluate it better. She smiled and said, "OK." Very polite and pleasant.
The CT scan showed about 9 different nodules and some enlarged mediastinal (middle of her chest) lymph nodes. This wasn't infection, this is most likely metastatic cancer. I went back to her room after talking to the radiologist to confirm my suspicians. I asked if she had ever smoked or worked in a factory. By this time, her daughter had arrived, and they both said, "No." But, then they admitted that Thelma's late husband had smoked all his life, and that all of the kids and in-laws smoked.
I explained that there were masses in her lungs, and that the mediastinal nodes could have been pushing on her esophagus causing the reflux-like symptoms and chest pain. I said I couldn't call it "cancer" because that's a tissue diagnosis, but that the nodules were suspicious for cancer. I told them I would be calling her doctor and making a plan.
After talking to him, and he was majorly surprised, I went back into the room and had to explain everything all over again to the son-in-law. He and her daughter both looked somewhat guilty when we talked about the possibility of second-hand smoke having caused her nodules. We sent them off with a referral to Roswell Park Cancer Center. Unfortunately, they're not connected to our system, so I don't know how I will be able to follow up, but I am sure I should be able to find some info.
Again, something so simple... and, I ended up giving this family some of the worst news you can share with a family. I hope they do well. They seem close. I certainly hope they are.
Labels:
lung cancer,
Roswell Park Cancer Center,
STEMI,
x-ray
18 November 2008
Monday Night Fights, Um, Football
 I think at some point I remember mentioning that, as part of our residency training, we learn to work at "mass gathering" events. I had a chance earlier in the year to go to the Bills vs. Raiders game, and yesterday I worked the Bills vs. Browns game where I probably spent about 75% of my time sewing up drunk fans or fans involved in altercations with drunk fans.
I think at some point I remember mentioning that, as part of our residency training, we learn to work at "mass gathering" events. I had a chance earlier in the year to go to the Bills vs. Raiders game, and yesterday I worked the Bills vs. Browns game where I probably spent about 75% of my time sewing up drunk fans or fans involved in altercations with drunk fans.It's strange, but I don't mind it. I like to suture. It's almost like artistry. You take something that's torn, or cut or shredded and try to put it back together. Of course, the majority of the suturing occurred on people's faces which leads to the added pressure of making sure that cosmetically suitable results are achieved. And, it doesn't matter that the majority of my patients were so sloshed they wouldn't have noticed if I sewed their top lip to their bottom eyelid; my own pride and perfectionistic attitude wouldn't allow me to accept anything but my best.
Now, having said that, it's a challenge to work on someone who's heavily intoxicated while remembering my Hippocratic oath. If you've never had stitches on your face, or seen someone getting them, it's a pretty intimate situation. Especially when I had two patients needing sutures inside of their mouths because they had cut the inside of their lips.
Beer breath is nauseating. Stale beer breath with cigarette tobacco overtones even worse. Of course, the fun patient of the night was the majorly drunk patient in handcuffs who was jumping and fighting the two sheriff's deputies who had him under arrest. The patient needed just one stitch. On his lip.
Ever try to wash a cat? Yeah, the two sheriffs holding him down looked something like that. To top it off, we didn't have a suture kit, and I was using what I had available... a suture removal kit. So, here I was trying to hold the needle with a pair of scissors and getting a stitch into a moving target.

The sheriffs managed to hold his head but couldn't keep him from talking. I guess I didn't think about the possibility of him spitting or kicking out. He managed to stop talking long enough for me to swoop in, throw the stitch, step back and then take another step forward as I quickly tied my knots and then cut the stitch. No lidocaine for him, but given his blood alcohol level, I don't think he even noticed.
OK, that's it for tonight. I need to write about my last patients at Suburban before starting back at the excitement that is ECMC. Grand Rounds tomorrow, so I should have some time to write... cheers! Of course, always in moderation... :)
Labels:
blood alcohol level,
Buffalo Bills,
laceration,
suture
15 November 2008
These Shoes are Made for Walkin'
 Sometimes you just have to buy something because it's so fun! Like these shoes. I now have 4 pairs of Dansko clogs which seem to be the shoes de rigeur amoungst the medical set. Wednesday was payday, so I went to my local outfitters to get a pair of black clogs for work.
Sometimes you just have to buy something because it's so fun! Like these shoes. I now have 4 pairs of Dansko clogs which seem to be the shoes de rigeur amoungst the medical set. Wednesday was payday, so I went to my local outfitters to get a pair of black clogs for work.I wanted a pair of black ones since I occasionally wear my clogs for quick trips to the market, or for meetings at the hospital, etc. When I went into the store, I saw these, and even though I am pretty conservative by nature I knew I had to get them. They are the same reliable comfortableness of all Dansko shoes, but just a little funkier.
You usually don't think much about your shoes until you are in them all day. And the last 2 shifts have been so hellish that I am glad to be wearing something solid and comfortable to carry me through those long 12 hour days. My colleague that was shopping with me asked what I would do if I spilled something on them, or had something (think biological material) drip onto them. I guess jump back and avoid the spill. I don't care, they're funky and cool as well as practical.
I think the nursing home floodgates opened up the last 2 days, and the ED seemed to be running a promotion on hospital admissions as my admit percentage ratio was around 75%. Last night I was 50/50 between admissions and discharges. There's just too many falls with hip fractures and chest pains to be evaluated. And, it's not even the beginning of pneumonia season yet.
Coming here this morning, I was thinking about how people don't realize that every single step of being seen in the E.D. takes time. You're triaged when you walk in the door. Triage - people who are sicker get to go first. And, you can't fake it. Vital signs don't lie. You can't say you have a high fever and then have a normal temp here. You can't say you can't breathe and then have a normal oxygen saturation on the pulse ox. Roll around on the floor saying you're having severe abdominal pain, and the triage RN will feel your soft stomach and know you're good for another couple of hours.
Then, you get into a room. First the aide takes your vitals. Then the RN does their exam. Then the M.D. gets the chart. After being interrupted by phone calls, bed hold orders, another nitro for the CP in 7, the M.D. will attempt to make it to your room. On the way, the psych patient in 13 will decide the walls are covered in bugs necessitating a B-52 (benadryl 50, haldol 5, ativan 2). When they finally return their second page out to the admitting attending for the patient in 22, the M.D. will make it to your room.
In my case, I then have to present to the attending that is managing all the other 20 patients in the E.D. along with 2 P.A.'s, a med student and another resident. So, I have to wait my turn. Finally, we decide on a plan, order labs, films, etc. I then place the order with the clerk who may or may not have called her kids for the 5th time to tell them that "no, you can't spend the night at Sally's because your father is going to be late and you need to watch the other two." When they finally get around to placing the order, if you have a film, you're again triaged behind the chest pains, the shortness of breaths, the other 10 abdominal pains, and the little old lady who fell over her walker while getting ice cream and now can't stand.
Two hours later when we have a second to look at the results of your labs, if they're all there and I don't have to be calling to lab to see what happened to them, or asking the RN or asking the aide who was supposed to have delivered them, but instead stopped to gossip in the stairwell with the cute guy from the third floor, I will finally see if I can figure out what's causing your _______.
Then I have to again talk to the attending, wait for your doctor to call me back, the consultant to call me back, the admissions' clerk to take the order and find you a bed, and the RN to finally send off the urine sample you haven't provided because you can't seem to hold the cup in the right spot, I might just come into the room to tell you I didn't find the reason for your abdominal pain, and I am going to discharge you to follow up with your primary care physician... which, might I say, you should have done in the first place since you've been having abdominal pain for the last 5 weeks, and tonight thought you should get it checked out because you saw a special on Oprah that talked about colon cancer.
I really should get a pedometer... I'm going to be getting a lot of mileage out of my new pair of shoes. Wait, first patient of the day... I know it won't be the last!
11 November 2008
Heal With Nerves of Steel
Suburban has been a really great experience. I am seriously enjoying my work there as I see a great variety of patients and diseases. However, a twelve hour long shift can be taxing, and on Sunday I was getting ready for my shift to be over... Since the board had been full all day, I was planning on seeing one more patient before ending my day, when the family practice resident I was working with asked if I wanted to swap patients.
She had just picked up an abscess case, and I was going to go see a woman coming in from another hospital with an "unusual finding on CT." I agreed as the abscess case could probably be finished before the end of my shift, and I wouldn't have to sign anything out. I am glad I did. I know comments have been made about doctors being the worst patients. However, I've found that working at Suburban, we seem to get a lot of families coming in with family members who are physicians, or nurses, or paramed ics, etc. They can cause us a lot of grief sometimes... but, more on that later.
ics, etc. They can cause us a lot of grief sometimes... but, more on that later.
My patient was a college student with an abscess on his tush. He'd already been to an urgent care center and had been prescribed antibiotics, but the abscess had just grown bigger. So it had be opened. Oh yeah. I have a friend from med student who once said that there was nothing more satisfying than draining an abscess, and I have to agree. Plus it meant I got to cut into someone and given the way the day had been going, I was more than eager to wield some steel.
After numbing the area, you basically make two incisions, "place the mark of Jesus on him" as my attending told me, and let everything drain out. I prepped the area, gave the patient adequate anesthesia and enjoyed the gushing, um, fruits of my labor. After exploring the abscess cavity to make sure there weren't any further pockets, I stuffed it full of packing. I then instructed the patient on wound care and told him to come back on Tuesday. I'll be working, so I hope I get to follow up on him.
When I came out of the room, it was like a war zone had set itself up in the E.D. First off, there was a patient found down that the EMT's decided to put onto the rig. Then when he was pronounced, they were obliged to bring the patient into the E.D. as they couldn't then remove the patient from the back of the ambulance. The family followed the patient to the hospital and soon there was the sound of crying and wailing throughout the E.D. At the same time, a family brought in a patient after chemotherapy. They were saying that the patient sometimes got a little "loopy" but this time they were much worse. So much so they were having a full out delirium and screaming and crying in their room. Then, the doctor family member of the patient I had traded the family resident with began demanding and belittling the staff to the extent that security had to be called.
The family medicine resident told me that when she explained to the family member that the attending was dealing with a patient coding (meaning CPR resuscitation) he stated, "That patient is probably dead and my wife is in pain. He should be here seeing her." Which went along with the family member of the delirious patient who kept following the RN's around asking that something be done about his family member. When my attending tried to explain that he had a patient that was sicker, and the family member didn't want to hear it, the quote was, "I have a patient who isn't breathing and this one still is, so I have to attend to them first."
I know it's hard to understand the system of triage when it's your loved one in trouble, and I can sympathize and apologize to patients when I go in to see them, but I can imagine with the change in leadership, things are just going to get worst. But, I will reserve getting on my soapbox for another time. It's late, and there's another shift in about 10 hours, so I better get to sleep. Will follow up on everyone. If there's a case in particular I've mentioned you'd want to hear about, let me know in the comments... We have to follow up on our cases, so I usually know what's happened to someone once they've left the E.D.
Until later... cheers!
p.s. other interesting cases during the shift: Bell's palsy in a 30 year old, an 80 year old runner who still walked 4 miles a day coming in with fulminant heart failure and not really having any symptoms, the 75 year old who went into sustained V-tach and needed to be shocked out of it, both of those patients had to be on amiodarone drips to keep their heart rates regular, and the 30 year old pregnant woman I got to reassure about her baby.
She had just picked up an abscess case, and I was going to go see a woman coming in from another hospital with an "unusual finding on CT." I agreed as the abscess case could probably be finished before the end of my shift, and I wouldn't have to sign anything out. I am glad I did. I know comments have been made about doctors being the worst patients. However, I've found that working at Suburban, we seem to get a lot of families coming in with family members who are physicians, or nurses, or paramed
 ics, etc. They can cause us a lot of grief sometimes... but, more on that later.
ics, etc. They can cause us a lot of grief sometimes... but, more on that later.My patient was a college student with an abscess on his tush. He'd already been to an urgent care center and had been prescribed antibiotics, but the abscess had just grown bigger. So it had be opened. Oh yeah. I have a friend from med student who once said that there was nothing more satisfying than draining an abscess, and I have to agree. Plus it meant I got to cut into someone and given the way the day had been going, I was more than eager to wield some steel.
After numbing the area, you basically make two incisions, "place the mark of Jesus on him" as my attending told me, and let everything drain out. I prepped the area, gave the patient adequate anesthesia and enjoyed the gushing, um, fruits of my labor. After exploring the abscess cavity to make sure there weren't any further pockets, I stuffed it full of packing. I then instructed the patient on wound care and told him to come back on Tuesday. I'll be working, so I hope I get to follow up on him.
When I came out of the room, it was like a war zone had set itself up in the E.D. First off, there was a patient found down that the EMT's decided to put onto the rig. Then when he was pronounced, they were obliged to bring the patient into the E.D. as they couldn't then remove the patient from the back of the ambulance. The family followed the patient to the hospital and soon there was the sound of crying and wailing throughout the E.D. At the same time, a family brought in a patient after chemotherapy. They were saying that the patient sometimes got a little "loopy" but this time they were much worse. So much so they were having a full out delirium and screaming and crying in their room. Then, the doctor family member of the patient I had traded the family resident with began demanding and belittling the staff to the extent that security had to be called.
The family medicine resident told me that when she explained to the family member that the attending was dealing with a patient coding (meaning CPR resuscitation) he stated, "That patient is probably dead and my wife is in pain. He should be here seeing her." Which went along with the family member of the delirious patient who kept following the RN's around asking that something be done about his family member. When my attending tried to explain that he had a patient that was sicker, and the family member didn't want to hear it, the quote was, "I have a patient who isn't breathing and this one still is, so I have to attend to them first."
I know it's hard to understand the system of triage when it's your loved one in trouble, and I can sympathize and apologize to patients when I go in to see them, but I can imagine with the change in leadership, things are just going to get worst. But, I will reserve getting on my soapbox for another time. It's late, and there's another shift in about 10 hours, so I better get to sleep. Will follow up on everyone. If there's a case in particular I've mentioned you'd want to hear about, let me know in the comments... We have to follow up on our cases, so I usually know what's happened to someone once they've left the E.D.
Until later... cheers!
p.s. other interesting cases during the shift: Bell's palsy in a 30 year old, an 80 year old runner who still walked 4 miles a day coming in with fulminant heart failure and not really having any symptoms, the 75 year old who went into sustained V-tach and needed to be shocked out of it, both of those patients had to be on amiodarone drips to keep their heart rates regular, and the 30 year old pregnant woman I got to reassure about her baby.
06 November 2008
So Much to Learn...
 Best quote of the night, "I heard that Obama got elected president, then I started to feel sick to my stomach, and then I just started throwing up."
Best quote of the night, "I heard that Obama got elected president, then I started to feel sick to my stomach, and then I just started throwing up."- 7 year old patient being seen for abdominal pain and vomiting
This is my newest cat Lacey, and some of you know that Lacey is deaf. I discovered it about 2 weeks after I got her when I realized that she wasn't reacting to the other 2 cats hissing at her even though they were mere inches apart. It was also just about the time she was finally over her upper respiratory infection from the stress of a new environment, and she started exploring around the apartment. Most cats will stop doing something at the sound of a loud clap or rustle of a newspaper, but Lacey didn't. I was trying to teach her her name and commands like I had Winston and Sofie, but she just didn't seem to get it.
Then there was the screaming. She would meow softly, then louder, then louder until it sounded like someone was twisting her tail off. And, that was when I was sitting in the same room. If she didn't see someone the scream was even louder. That's when I realized that she might be deaf. I went online and started researching what to do with a deaf cat. My husband laughed when I told him we were now parents of a "special needs" child. Still it's been a learning process for me and Lacey. One of the articles I came across talked about teaching your cat sign language. Given my schedule, it's been a challenge to be consistent, but she's still able to tell me what she needs. And, since she's attached h
 erself to my male cat who is more tolerant of her, the screaming is limited to when she doesn't see him in the room when she wakes up.
erself to my male cat who is more tolerant of her, the screaming is limited to when she doesn't see him in the room when she wakes up.I bring this up, because Lacey has taught me how something so simple could become so complicated. I wanted a new cat, I thought it was time. I went to the Humane Society multiple times over the course of about a month to pick out just the right kitten to bring home.
They say that you don't pick your cat, your cat picks you, and it was fated the way I ended up with her. I was casually talking to the volunteer about when they might get some more kittens in, and we were walking by the older adult cat cages. I had briefly noted that her tag read 5 months old without even really looking at her, and I asked about cats making adjustments with adding an older cat.
The volunteer and I stopped and talked in front of Lacey's cage for a while, and it was during that time that I finally took a look at her. She was just about what I wanted with her longer fur and black coat. On a whim, I asked if I could see her and took her to the cat room. She started purring and walking around the room curiously exploring. I didn't think much about the fact that she wouldn't come when called. She was a stray. But, the more I sat with her, the more I really liked her. Then she did the ultimate. I asked if she wanted to go hom
 e with me and she fell on the floor in front of me and did the feet in the air upside down glance. I was hooked.
e with me and she fell on the floor in front of me and did the feet in the air upside down glance. I was hooked.I think about her while I am at work. How the simplest thing can become so complicated so easily, and how I have so much still to learn.
I picked up a chart yesterday that read "vaginal bleeding." Now, I knew this meant doing a pelvic, which I've talked about extensively, so you know my feelings on that, but I figured it would be quick and easy. Not so much. Following a surgical procedure on her cervix, this patient developed a condition which is common 10 - 14 days later which could cause her to bleed to death. As soon as I started my exam, I knew something was wrong, and I called my attending into the room. My patient ended up going emergently to the OR. I will find out what happened to her when I go back tomorrow.
I had another patient who woke up this morning feeling as though the room was spinning. I can tell you there were a lot of college nights I felt the same, but that's another story. He lay back down and then tried again a few minutes later and the room continued to spin. He tried to sit up and then started feeling so nauseated he had to lie down again. That's when he woke up his wife who called 911. Something simple - vertigo, however his blood pressure was 260/140. Not so simple. There's a condition where you can have a stroke or bleed in the cerebellar part of your brain which leads to these exact symptoms. He was rushed to the CAT scan almost as soon as he arrived and was stabilized. He was transferred to our stroke center Gates Hospital within about 1/2 hour after he arrived. I will be checking on him too.
I am still adjusting to life with a deaf cat. She knows finger pointing at door means go through it and out. And, about 75% of the time she actually does it. We're both still learning.
Labels:
cerebellar bleed,
cervical bleed,
deafness,
Lacey,
LEEP procedure
02 November 2008
Back from Chi-Town!
Oh what a trip! I can't believe in 5 years how much has changed.
Although I was there for the conference, I really wish that I'd had more time to explore my old neighborhood. My driver back to the airport had actually grown up in the neighborhood where I lived while an intern, and he and I talked about all the changes that Chicago has seen. Like everywhere else, Chicago is being affected by the economy, and we talked about the projects started and not yet complete.
Anyway, on Sunday we had the med student Residency Fair where I was able to share our program with perspective applicants. I was able to meet a lot of people from a variety of programs and hopefully sell them on coming out to Buffalo to interview. We then checked into our hotel and hit one of my favorite spots for Chicago style deep dish pizza - Edwardo's!
I was worried for a sec, because a number of buildings along the street were torn down, but we turned the corner, and there it was! The sauce is still thick, the cheese even thicker and the spinach and mushroom filling, still fresh. Yummy! My colleague thoroughly enjoyed it as well. This one is off Congress, on a street just west of State across from the Chicago Public Library. I remember flying a frozen pizza back to California just to share the taste with my family. Oh, yeah.
During the rest of the week, our days were filled with meetings, our nights with going to different restaurants and having way too much fun! I passed Garrett's several times while out, but I was never able to actually make it into the store. Plus, that large poster board on the table, yeah, I had to carry that on the plane. They wanted to charge me for an extra carry-on which I was able to avoid going to Chicago, so I opted out of stopping at Garrett's to bring back a tub of their popcorn which would have been too much for the trip back. :( Next time.
The conferences ranged from boring to interesting, and it is very exciting to hear what is happening in other parts of the country. While Buffalo is just setting up their hypothermia protocol for post-cardiac arrest patients, other parts of the country, ie: U of Pittsburgh are writing and publishing their results. We have hundreds of possible lectures to choose from, and I chose all the ones I thought would help me at this stage in my career - mostly dermatology and cardiology topics.
However, I did go to some fun ones like "1001 Uses for Duct Tape and a Safety Pin." It was taught by an attending who does Wilderness Medicine, and who shared photos and stories of his travels all around the world. He works sometimes at the clinic on the road up to Mount Everest, and the stories he told about saving lives with just the basics are amazing. I left the meeting both inspired and humbled. There's so much to learn.
I was also very excited to see some friends from medical school who I hadn't seen since graduation and who are now attendings in different parts of the country. It was kind of funny to explain to them that I was still a resident, but we all follow different paths. I exchanged addresses and emails with them. A whole new set of connections.
Finally it was time to come back home to my current world. The children behaved, and my apartment seems to be intact. I worked yesterday and am starting a stretch of nights tonight. Will be exciting to see what I can apply from the conferences I attended this last week just as it is exciting to be contemplating my future...!
Subscribe to:
Posts (Atom)